November 2023
On Jan. 1, 2023, Blue Cross and Blue Shield of Oklahoma created a new network called MyBlue HMO.
What are some requirements of the MyBlue HMO Member Health Plan?
*The PCP can be a family practitioner, pediatrician, internist, or physician assistant or advanced practice nurse in one of those areas of practice.
The MyBlue HMO PCP can be an independent provider or one from the following provider groups:
Counties |
Provider Groups |
Cleveland, Lincoln, Logan and Oklahoma |
|
Creek, Okmulgee, Osage, Pawnee, Rogers and Tulsa |
|
The following hospitals can be used with a referral from MyBlue HMO Member’s PCP through BCBSOK in addition to the MyBlue HMO Member’s specialist:
Counties |
Hospitals |
Cleveland, Lincoln, Logan, and Oklahoma |
|
Creek, Okmulgee, Osage, Pawnee, Rogers and Tulsa |
|
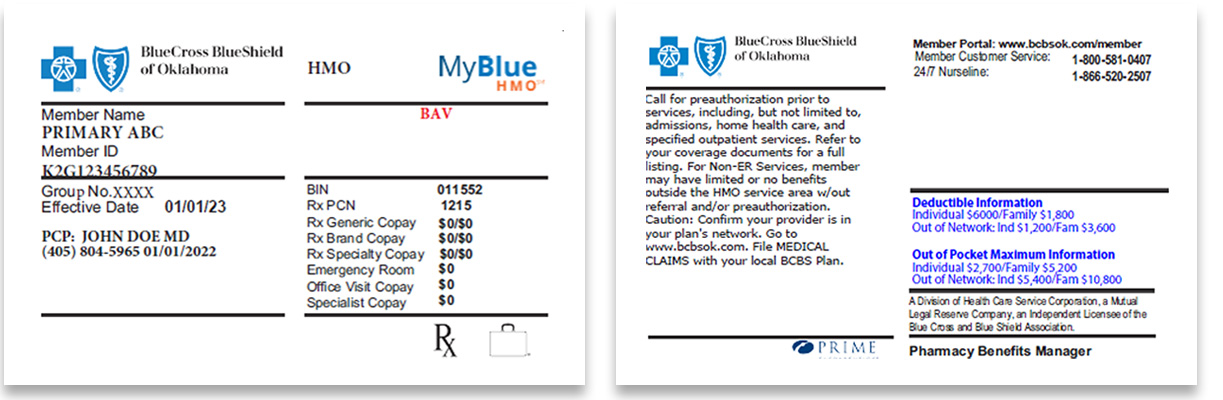
How can I identify MyBlue HMO Members?
MyBlue HMO Members are identified by the following on their BCBSOK ID card:
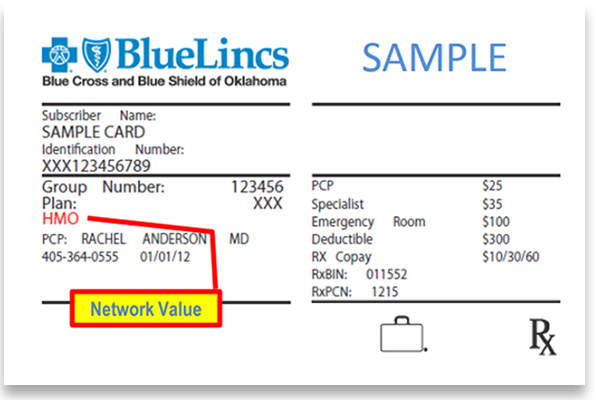
How can I identify a MyBlue HMO Member from a BlueLincs HMOSM Member?
BlueLincs HMO Members are identified by the following on their BCBSOK ID card:
 ;
;
How can I verify eligibility and benefits for MyBlue HMO Members?
Providers should verify eligibility and benefits prior to every scheduled appointment through Availity® Essentials or your preferred web vendor. Eligibility and benefit quotes include participant confirmation, coverage status and other important information, such as applicable copayment, coinsurance and deductible amounts. When services may not be covered, participants should be notified they may be billed directly.
How can a MyBlue HMO PCP obtain a required referral?
If the MyBlue HMO Member’s assigned PCP is not available, is a referral required for the MyBlue HMO Member to see another MyBlue HMO PCP?
If the MyBlue HMO PCP is located at the same physical address as the Member’s assigned PCP or has the same tax ID, then no referral is required.
Do emergency services require a referral?
Yes, the MyBlue HMO PCP is required to obtain a referral within two (2) business days of the emergency department visit or inpatient hospital admission.
What happens if the required referral is not obtained?
Failure to obtain the required referral may result in services being denied.
If you have questions, please contact your Provider Network Representative.