Oct. 25, 2023
Reminder: New Medicare Supplement Enrollment Requirements
Effective Sept. 1, 2023, the Oklahoma Insurance Department amended the Medicare Supplement regulations and created new enrollment requirements.
OAC 365:10-5-129(f)
Amendments to Oklahoma Administrative Code (“OAC”) 365:10-5-129(f) create new enrollment opportunities for Medicare supplement policyholders. The regulation requires Medicare supplement issuers to provide new supplement policies with the same or lesser benefits to current Medicare supplement policyholders — regardless of current issuer — who have had no gap in coverage greater than ninety (90) days since initial enrollment. Medicare supplement issuers that provide these policyholders a sixty (60) calendar day “open enrollment” period beginning on the policyholder’s birthday each year, shall be deemed in compliance with this rule. Previously, these policyholders have had no opportunity after initial enrollment to move to any other Medicare supplement policies or issuers, trapping the policyholders in policies with rising premium costs and no opportunity to search for lower premium rates.
Issuers offering a new (i.e., succeeding) supplement policy shall waive medical underwriting or preexisting exclusions if the new supplement policy offers the same or lesser benefits. Issuers of the current (i.e., prior) policy are required to furnish a statement of benefits or other pertinent information sufficient to permit verification of benefit determination to any new issuer upon request. ![]()
If an applicant is applying to Medicare Supplement from a different carrier, they need to select “Yes” on Question #5 and complete part 5a indicating the name of the carrier and plan. Once the application is submitted, the individual will be contacted by BCBSOK Customer Support regarding the applicant’s Term Date of their prior Medicare Supplement coverage to ensure there is not more than a 90 day gap in coverage. To avoid a delay in processing, please include prior carrier, prior plan, and term date of that plan on the line provided under question 5a.
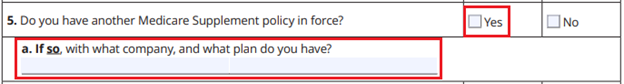
Note: The Retail Producer Portal, Blue Access for ProducersSM, The Retail Shopping Cart and Sales Force will not recognize the ‘birthday rule’ or the other rules associated with the OID bulletin. so agents will still be prompted to answer these questions If the agent knows the applicant is ‘Guarantee Issue,’ they do not need to answer the ‘Health History’ questions.